Artificial Intelligence in Retinal Diseases: A Focus on Age-Related Macular Degeneration (AMD)
AI in Retinal Disease: A New Era for AMD Diagnosis & Treatment
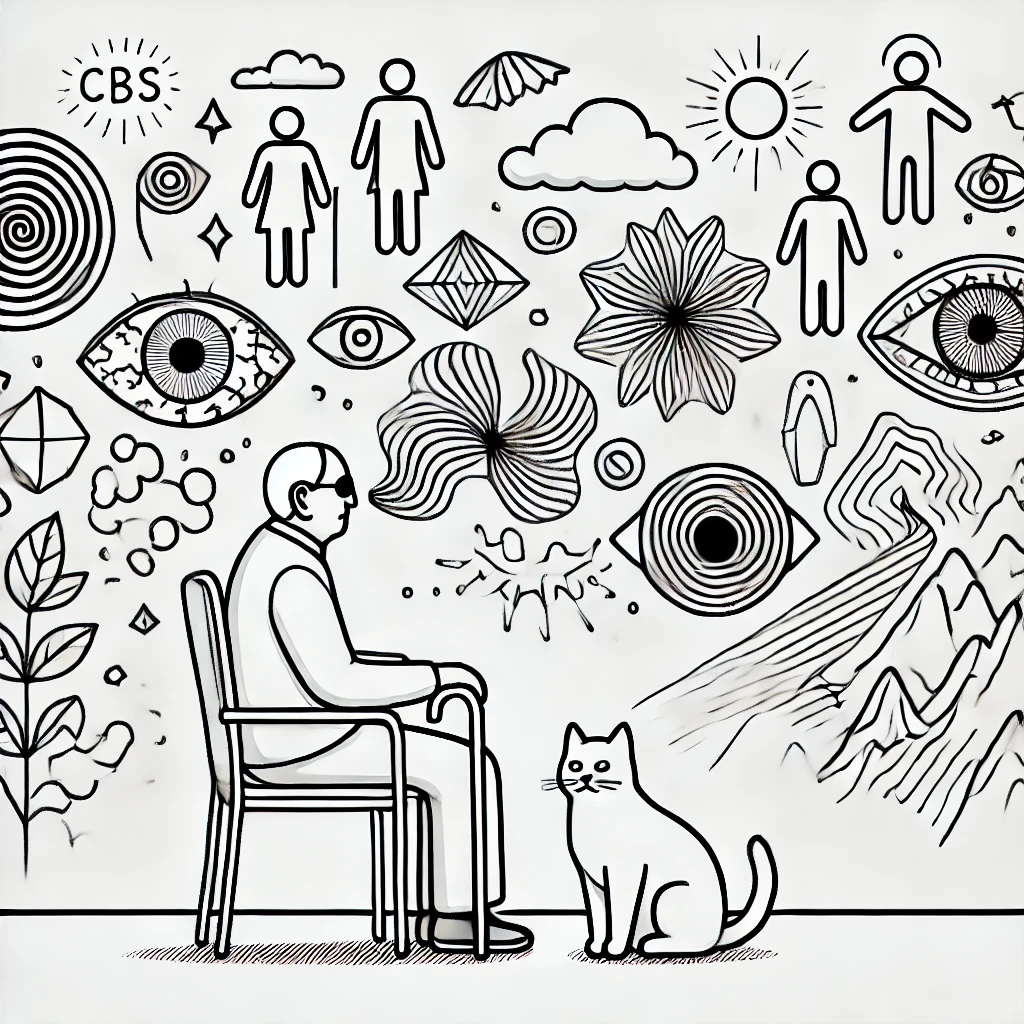
Abstract Artificial intelligence (AI) is revolutionizing ophthalmology, particularly in the diagnosis, prognosis, and management of retinal diseases. Age-related macular degeneration (AMD), a leading cause of blindness, has benefited significantly from AI-driven approaches for early detection, risk assessment, and personalized treatment. This review synthesizes recent advances in AI applications for retinal diseases, with a particular focus on AMD, covering automated diagnosis, predictive modeling, AI-assisted treatment strategies, and telemedicine integration. The review also discusses the challenges of AI implementation, including algorithmic bias, interpretability, and regulatory concerns, and provides insights into future directions for AI-driven ophthalmic care.
1. Introduction
Retinal diseases, including diabetic retinopathy (DR), glaucoma, and AMD, are leading causes of vision impairment worldwide. With AMD expected to affect 288 million people by 2040 [1], the demand for advanced diagnostic and treatment tools is increasing. Traditional diagnostic methods, such as optical coherence tomography (OCT) and fundus photography, rely on human interpretation, which can be subjective and time-consuming. The integration of AI, particularly deep learning (DL) and machine learning (ML), has significantly improved early detection, disease monitoring, and treatment planning in AMD and other retinal diseases [2-5].
Additionally, AI facilitates better workflow efficiency in clinical settings by automating image interpretation and disease classification, thus reducing the burden on specialists. The scalability of AI models allows for widespread deployment in screening programs, particularly in underserved and remote areas. With continual advancements, AI is expected to become an indispensable tool in retinal disease management.
This review explores the latest AI applications in AMD, including AI-powered image analysis, predictive modeling for disease progression, AI-guided anti-VEGF therapy, and telemedicine solutions. The challenges and ethical considerations in AI adoption for clinical practice are also discussed.
2. AI in Retinal Disease Diagnosis
2.1 Deep Learning for Image-Based Diagnosis
AI models, particularly convolutional neural networks (CNNs), have demonstrated high accuracy in analyzing fundus photographs and OCT scans for retinal disease detection. Studies have shown AI can classify early, intermediate, and late AMD with over 90% accuracy [6-9]. Telemedicine integration has allowed AI-based remote screening, improving access to eye care in underserved areas [10-12].
Moreover, AI-driven automated screening tools are capable of flagging abnormalities in real-time, leading to faster referral decisions and timely intervention. These tools enhance diagnostic precision by minimizing observer variability, which is a common challenge in manual image interpretation. The use of multimodal imaging, where AI combines OCT and fundus photographs for enhanced accuracy, further strengthens its role in early disease detection.
2.2 AI-Augmented OCT Analysis
OCT imaging remains the gold standard for AMD diagnosis. AI-enhanced OCT segmentation facilitates:
- Automated detection of drusen, an early AMD biomarker [13-16].
- Fluid quantification in wet AMD, optimizing anti-VEGF treatment decisions [17-19].
AI-assisted OCT interpretation has demonstrated diagnostic performance comparable to expert ophthalmologists [20-22]. Additionally, AI models can analyze volumetric changes over time, providing insights into disease progression and treatment response. This enables ophthalmologists to make more informed decisions on therapeutic strategies.
3. AI in AMD Prognosis and Risk Prediction
Predicting AMD progression is essential for early intervention and treatment monitoring. Machine learning models can:
- Predict transition from dry to wet AMD using retinal biomarkers and genetic markers [23-25].
- Forecast geographic atrophy progression based on longitudinal OCT datasets [26-28].
- Provide personalized risk assessment integrating AI with genetic factors [29-31].
These predictive tools enable earlier interventions and tailored patient monitoring. AI-based progression models leverage vast patient datasets to identify patterns that may not be apparent through conventional analysis, leading to more individualized disease management plans.
4. AI for Treatment Optimization
4.1 AI-Guided Anti-VEGF Therapy Personalization
Anti-VEGF injections are the primary treatment for wet AMD, but response varies. AI models assist by:
- Predicting treatment response, optimizing injection intervals [32-35].
- Reducing overtreatment and minimizing patient burden through optimized dosing regimens [36-38].
AI-assisted treatment planning has led to improved visual outcomes and reduced healthcare costs [39-41]. Additionally, AI can help stratify patients into responder and non-responder groups, allowing for more targeted therapy and reducing unnecessary treatments. Future advancements may integrate AI with wearable biosensors for real-time disease monitoring.
4.2 AI-Enabled Disease Monitoring
AI-powered OCT analysis provides real-time assessment of treatment efficacy, enabling earlier detection of recurrence in wet AMD [42-44]. Emerging AI-based home OCT imaging tools allow patients to track disease progression remotely, improving treatment adherence and outcomes [45-47].
These home monitoring systems empower patients by offering proactive disease management while reducing the need for frequent in-person visits. The combination of AI and remote monitoring ensures that interventions are initiated at the optimal time, potentially preventing severe vision loss.
5. Challenges and Limitations
Despite promising advances, AI adoption in ophthalmology faces significant hurdles:
- Algorithmic Bias: AI models trained on homogeneous datasets may perform poorly in diverse populations [48].
- Lack of Explainability: The "black-box" nature of deep learning raises clinical trust concerns [49].
- Regulatory Barriers: AI-based medical devices require extensive validation before clinical integration [50,51].
Moreover, data privacy concerns and ethical implications surrounding AI-driven decision-making remain areas of active discussion. Addressing these issues is crucial for fostering clinician and patient trust in AI-based ophthalmic solutions.
6. Future Directions
The future of AI in AMD and retinal diseases includes:
- Multi-ethnic AI training datasets to improve generalizability.
- AI-augmented telemedicine for expanding remote AMD screening.
- AI-powered drug discovery for novel neuroprotective treatments.
Further research is needed to bridge AI innovations with real-world clinical applications. The potential of AI to integrate genomic data with imaging biomarkers holds promise for even more personalized approaches to AMD care.
7. Conclusion
AI has transformed retinal disease management, particularly for AMD. Deep learning models enable automated diagnosis, predictive analytics enhance risk assessment, and AI-driven treatment personalization improves patient outcomes. Despite challenges, AI-driven ophthalmology holds immense potential for revolutionizing AMD care, making early detection and personalized treatment more accessible than ever.
Future developments in AI and ophthalmology will continue to refine diagnostic accuracy, improve treatment efficiency, and enhance patient outcomes. As technology advances, AI will play an increasingly central role in preventing and managing vision loss worldwide.
References
1. Br J Ophthalmol. 2020 April ; 104(4): 449–450. https://pmc.ncbi.nlm.nih.gov/articles/PMC8330345/
2.Fatima T, et al. Intelligent Decision Technologies 18 (2024) 1695–1710 1695; https://journals.sagepub.com/doi/10.3233/IDT-241007
3.Burlina P, et al. JAMA Ophthalmol 2017 Nov 9;135(11):1170–1176. https://jamanetwork.com/journals/jamaophthalmology/fullarticle/2654969
4. https://pubmed.ncbi.nlm.nih.gov/30104768/
5. https://iovs.arvojournals.org/article.aspx?articleid=2561941
6.https://doi.org/10.1038/s41598-020-72359-y
7.Comput Biol Med. 2017 March 01; 82: 80–86. https://pmc.ncbi.nlm.nih.gov/articles/PMC5373654/pdf/nihms849294.pdf
8.JAMA Network Open. 2022;5(5):e229960. https://pmc.ncbi.nlm.nih.gov/articles/PMC9066285/
9. https://doi.org/10.1007/s00417-023-06052-x
10. https://doi.org/10.1016/j.ophtha.2018.02.037
11. https://doi.org/10.1016/j.eclinm.2021.100875
12. Eye (2023) 37:2438–2453; https://doi.org/10.1038/s41433-022-02360-4
13. https://pmc.ncbi.nlm.nih.gov/articles/PMC6810830/
15. Gao Y, et al. BMJ Open Ophth 2024;9:e001903. https://pmc.ncbi.nlm.nih.gov/articles/PMC11580293/pdf/bmjophth-9-1.pdf
16. Novel Approaches for Early Detection of Retinal Diseases Using Artificial Intelligence
17. Artificial intelligence for diagnosing exudative age-related macular degeneration - PubMed DOI:10.1002/14651858.CD015522.pub2
18. JAMA Ophthalmol 2018 Sep 14;136(12):1359–1366. https://pmc.ncbi.nlm.nih.gov/articles/PMC6583826/
19. Crincoli et al. BMC Ophthalmology (2024) 24:121 https://doi.org/10.1186/s12886-024-03381-1
20. The future application of artificial intelligence and telemedicine in the retina: A perspective - PMC
21. Taiwan Journal of Ophthalmology 13(2):p 133-141, Apr–Jun 2023. https://pmc.ncbi.nlm.nih.gov/articles/PMC10361422/
22. https://assets.bmctoday.net/retinatoday/pdfs/0421RT_Cover_Alauddin.pdf
23. https://pmc.ncbi.nlm.nih.gov/articles/PMC8525840/
24. Integrating AI with tele-ophthalmology in Canada: a review - Canadian Journal of Ophthalmology
25. https://pmc.ncbi.nlm.nih.gov/articles/PMC11052176/
26. Impact of artificial intelligent and industry 4.0 based products on consumer behaviour characteristics: A meta-analysis-based review - ScienceDirect
27.https://www.sciencedirect.com/science/article/pii/S2162098923002104?via%3Dihub
28.https://linkinghub.elsevier.com/retrieve/pii/S0002939406013274
29. https://doi.org/10.1590/1516-3180.2021.0713.R1.22022022
30. https://doi.org/10.1016/j.infoh.2024.05.003
31. https://doi.org/10.1093/pnasnexus/pgab003
32. Ophthalmol Retina. 2022 February ; 6(2): 116–129. https://doi.org/10.1016/j.oret.2021.06.010
33. https://pmc.ncbi.nlm.nih.gov/articles/PMC7153739/pdf/nihms-1549995.pdf
34. https://pmc.ncbi.nlm.nih.gov/articles/PMC9240537/pdf/IJO-70-1140.pdf
35. https://doi.org/10.1016/j.ophtha.2018.11.015
36. Diagnostic accuracy of current machine learning classifiers for age-related macular degeneration: a systematic review and meta-analysis | Eye
37. https://pubmed.ncbi.nlm.nih.gov/27701631/
38. https://pmc.ncbi.nlm.nih.gov/articles/PMC10361422/pdf/TJO-13-133.pdf
39.https://bmcophthalmol.biomedcentral.com/articles/10.1186/s12886-024-03381-1
40.https://pmc.ncbi.nlm.nih.gov/articles/PMC7453007/pdf/41746_2020_Article_317.pdf
41.https://pmc.ncbi.nlm.nih.gov/articles/PMC6831476/pdf/thnov09p7556.pdf
42.https://assets.bmctoday.net/retinatoday/pdfs/0421RT_Cover_Alauddin.pdf
43. https://pmc.ncbi.nlm.nih.gov/articles/PMC8525840/
44. https://doi.org/10.1016/j.apjo.2024.100096
45. https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(23)00037-2/fulltext
46. Integrating AI with tele-ophthalmology in Canada: a review - Canadian Journal of Ophthalmology
47. https://pmc.ncbi.nlm.nih.gov/articles/PMC11052176/
48. https://pmc.ncbi.nlm.nih.gov/articles/PMC10169139/
49. https://pmc.ncbi.nlm.nih.gov/articles/PMC10361422/
51. https://bmcophthalmol.biomedcentral.com/articles/10.1186/s12886-024-03381-1
How is AI used in diagnosing age-related macular degeneration?
Can artificial intelligence predict AMD progression?
AI in ophthalmology: How is it transforming AMD treatment?
What are the latest AI advancements in AMD diagnosis?
Can deep learning improve age-related macular degeneration detection?
AI-powered retinal disease diagnosis: What’s next?
How does machine learning help in AMD treatment personalization?
AI-assisted OCT analysis for macular degeneration: How does it work?
Can AI replace ophthalmologists in AMD diagnosis?
The role of artificial intelligence in preventing vision loss from AMD
How does AI optimize anti-VEGF therapy for AMD patients?
What are the benefits of AI-powered telemedicine in AMD care?
AI in retinal imaging: What’s the impact on age-related macular degeneration?
Challenges and limitations of AI in AMD management
Future of AI in ophthalmology: Will it revolutionize AMD treatment?
AI-driven risk assessment for age-related macular degeneration
How AI home monitoring tools are improving AMD patient care
The ethical implications of using AI for AMD diagnosis
How AI is improving early detection of wet and dry AMD
Will AI-based drug discovery lead to new AMD treatments?

Leave a comment
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.